This article originally appeared in Southern Exposure Vol. 13 No. 2/3, "Older Wiser Stronger: Southern Elders." Find more from that issue here.
Madison County, North Carolina is rugged country. Its steep mountains, winding roads, and remote hollows have fostered a people who place a high value on strength, self-reliance, and traditional ways of doing things.
Many changes have taken place during the lives of the county's eldest residents; not least have been changes in health care. Reliance on home remedies and occasional doctors' visits may have given way more slowly in the mountains than in many other areas, but it has given way. The area now has modern clinics, home health nurses, family care homes, and an intermediate and skilled care nursing home.
The elderly in the county and their families, like people everywhere, want to retain as much control of their lives as possible. For most that means staying in their own homes, with familiar surroundings and routines. But a combination of factors is making that increasingly difficult.
One factor is the changing nature of the economy. Madison is traditionally a rural area where farm families have eked out a living from the rocky soil. Now less than 10 percent of the county's labor force makes a living farming, down from 70 percent or more just a few decades ago. Family farms lie fallow, and many have been bought for use as vacation homes as the younger generations move away in search of wage-earning employment.
Madison County women used to work the fields, raise gardens and small livestock, rear children, and provide three meals a day for work-fueled appetites. But today, fewer working forms, hard economic times, and changing social values mean that women as well as men are going into "public jobs." Over half of the women over 16 in the county now work outside home and farm. Since jobs are scarce in Madison, more than a third of the labor force commutes to adjacent counties or across the state line into Tennessee. The relatives and neighbors who once rallied to help when the sick or the elderly needed full-time care are now either living elsewhere or leaving home at dawn to drive long distances to work. As a result, the support system that once allowed older relatives to live out their lives at home has thinned.
Government regulations and private health care insurance rules throw up additional barriers. Medicare, the health insurance portion of the Social Security program, provides money for hospital care and visits to doctors or dirties. It will pay for visits from home health nurses only if a patient has been hospitalized, and then for only 20 days after release. Medicaid may then kick in to cover home health nurse visits if a patient can meet the stringent eligibility guidelines.
But neither Medicare, Medicaid, nor most private insurance programs pay anything for maintenance visits — for blood pressure checks, monitoring of diabetes or heart conditions, or any kind of routine health care that could help keep an older person mobile by providing medical attention before ailments become severe. Nor do those programs pay for choreworkers, home-delivered meals, or other support systems to help the elderly stay at home.
"We can get them well through home health, but then we are forced to leave, and then no one's there to monitor them," says Monica Teutsch, executive director of the Hot Springs health program, which operates the county's two clinics and home health nurse service. This makes no sense, she believes, even from a strictly economic viewpoint: "I'm personally convinced that just in saving inappropriate hospital visits, we could pay for a program of maintenance visits." Without skilled observation, chronic conditions that plague many older people flare up and go untreated. "Then a neighbor goes in and finds them in such a degenerated condition that they have to be hospitalized. A monthly visit by a nurse could keep that from happening."
An additional problem with Medicaid exists in areas where families are tied to the land. Most Madison County farms are larger than allowed as a homestead exemption under Medicaid eligibility rules; and after six months in an institution, the patient loses even that minimum exemption. For many of the elderly, family land is their inheritance, the product of a lifetime's work, and the intended legacy for future generations. They resist losing both the product of their labors and the link between past and future that the land represents.
Even if families decide to sell, they find that the market is slow for steep, isolated farms, and "fair market value" as rather arbitrarily defined by Medicaid regulations may be impossible to get. And for their failure to obtain it they are penalized by those same regulations in two ways. First, should they attempt to turn land over to its intended inheritors they may be declared ineligible for benefits for a full year. Second, if those intended beneficiaries wish to purchase the land, they must meet the "fair market value" standard. In a county where 45 percent of the households have incomes under $10,000, that is frequently impossible. Such regulations favor the urban and landless poor and have given rise to the notion in rural areas that if you go to the government for assistance, "they will take your land." There are no statistics available on the numbers of rural elders who do not seek help because of such fears.
"Folks work all their lives to build a home, and then when they get to the point where they want to be comfortable and enjoy what they've worked for they can't, and that's a shame," Teutsch says.
Recent cuts in federal funds for social programs have resulted in more stringent eligibility requirements so that fewer people qualify for the limited services still available. Remaining funds have lost ground to inflation and needed new services cannot even be considered. While some services are still available, most are underfunded and spread too thinly to meet the needs of the elderly.
The Hot Springs health program's two clinics and home health care service operate on a fee-for-service basis, with a sliding scale based on income, which is subsidized by grant money through federal programs. In 1984, the program's two registered nurses made nearly 3,000 home visits, mostly to elderly patients; 87 percent of those patients visited received some assistance through Medicaid or Medicare, and 92 percent of the rest were eligible for discounts. Since the fall of 1984, the service has expanded, adding another nurse, several nurses' aides, and a "Lifeline" service. Lifeline, which provides a monitoring device that allows a patient to call for emergency help by pushing a button attached to the clothing, is not covered by Medicare or Medicaid.
Also new in Madison County is an experimental long-term-care screening program through the Department of Social Services. Director Anita Davie says that the goal is to help people stay at home — even those who need regular medical attention. Patients who are accepted into the program can receive up to $1500 per month for aid not ordinarily covered by Medicare or Medicaid, such as maintenance health visits from nurses and aides, delivered meals, choreworkers, and minor renovations to adapt homes to people's physical limitations. "We can keep them at home cheaper than in a nursing home, or at least at no more expense," says Davie. "We may find it really is as expensive, but home is where they want to be."
Other agencies or organizations offer transportation to a doctor's office or clinic, hot lunches five days a week at seven nutrition sites, home-delivered meals, choreworkers to help do housework, and emergency money for fuel to help head off chill-related health problems. All these services are contingent on federal and state aid, and no one is ready to predict how far proposed new cuts will slice into them.
Whatever the sources of help, sometimes staying at home is impossible. Until a few years ago, leaving home for most elderly people meant leaving the county. Now Madison has five family care homes, each able to house up to six people needing housekeeping help but not full-time nursing care, and Madison Manor, a private for-profit intermediate- and skilled-care nursing facility with 100 beds. Those working with the elderly and their families say that Madison Manor has built a good reputation in the county and has made acceptance of institutional care easier.
Dr. Chipper Jones, one of the Hot Springs health program physicians, says that institutional care is often the best solution for patients who need around-the-clock care, and that families shouldn't feel guilty when they can no longer meet the needs of a patient at home. At Madison Manor many of the staff are local residents, the facility is close enough to allow frequent visits by relatives and friends, and many of the current residents are friends and neighbors of incoming patients. All these factors help to maintain the feeling of community so important to the county's residents.
But neither the quality of care nor the neighborhood atmosphere of Madison Manor has removed the stigma associated with institutional care, and resistance to "putting someone away" remains strong.
"Senior citizens in this area came through the Depression, and they're used to hard times," explains Edwin Phillips, who administers programs for the elderly within the Department of Social Services. "They stay home even if it means doing without. They just tighten their belts."
Their relatives, by and large, support that effort. Most still bristle at suggestions that their parents might be better off somewhere else. "We take care of our own," they insist proudly.
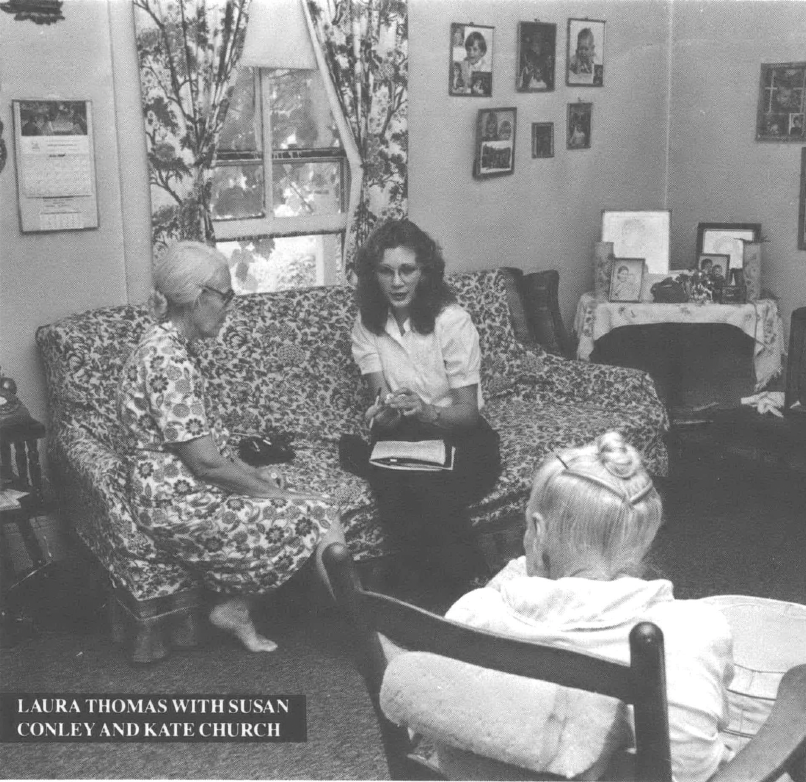
Laura Thomas has taken care of other people most of her life. She quit school at an early age to help support her family by caring for elderly neighbors. She later married and raised five children of her own. Now widowed, she has full responsibility for her mother, Kate Church, who's "about 100, I think, but nobody really knows."
Although Kate Church can eat without help and can move around on her own, she still needs someone with her constantly because of her weakened heart. One day a week, a neighbor comes in to stay with her so Laura Thomas can get out — usually to work in the garden. A home health nurse comes in periodically to take Church's blood pressure and check her heart. If that service were not available, the alternative would be expensive and time-consuming trips to the Hot Springs Health Clinic, trips Thomas says her mother finds confusing and tiring. A generation ago, when Thomas was growing up and health care consisted almost solely of home remedies, they wouldn't have had the option.
Thomas remembers the first time she went to a doctor, at age 13. She also remembers the treatment — a bottle of cod liver oil. The first dose came straight back up, the second she poured out when no one was looking. She got better anyway, and while she appreciates the advantages of modern medicine for those who need it, she says, "I'm not a person to run to doctors every time I have a pain. I don't have time; if I get sick, I just keep going."
At 70, Laura Thomas still raises a garden, cans, puts up pickles, and keeps a spotless house. Last year she cut her own firewood with a handsaw and tilled the garden herself. But now her youngest son is threatening to hide both tiller and saw unless she lets him do the heavy jobs for her. "I told her and told her and told her to leave the tiller alone," he says, half boasting, half concerned. "I've caught her several times over next door where she has her garden, a'plowing away. I told her I'm going to take the parts off it and take it home with me, and then I'll know she can't use it." Thomas just smiles; she's had this discussion before.
She refuses to consider a nursing home for her mother as long as she can handle care at home. Her son is just as strongly opposed to nursing home care for her should she reach the point where she couldn't care for herself. "She would be living with me and my wife," he insists.
"The way I feel about it," counters Thomas softly, "I just don't want to be a burden to nobody." She has a solution, though, spawned from years of caring for others : "If something happens to Mother before it does to me, I think I'll just go and get a job in a nursing home."
"Susan comes here, and she just takes over like she was one of the family."
It's the highest compliment Walter and Gertie Randall can pay to Susan Conley, the home health nurse who comes every other week to care for Gertie's father, George Roberts, age 92. Conley provides not only skilled nursing care, the Randalls say, but also a friendly ear and a willing hand. "She's even told me to call her on her day off if I just need someone to stay with him so I can get out," Gertie says.
That's the kind of help traditionally offered by family members and concerned neighbors. But the Randalls' seven children live miles away, or have jobs that mean fewer free hours. The full-time care George needs keeps Gertie homebound while Walter finds his way through unfamiliar tasks like grocery shopping. "I don't mind staying home," says Gertie. "I'd only call someone if it was a have-to case. If we didn't have Susan, I just don't know what we'd do. You get to thinking about it, what would anybody do? Back years ago, neighbors would come in and sit of a night, but you see there's just nobody around to do that now. Most everybody's working, and there's just nobody to help."
George Roberts spends much of his time sitting, sometimes smoking his pipe, occasionally joining in conversation with visitors, although his diminished hearing makes that difficult. "He's no trouble," Gertie says, watching her father sit quietly. "Most of the time, he's just like that." Conversation tends to be about her father more than with him. Questions to him, because they must be yelled, often become simplistic, as though spoken to a child: "How do you like Susan? Does she take good care of you?"
The answers are, as the questions deserve, short and simple. "I like her. Yes." As talk continues around him, Roberts is briefly quiet again. Then a wry humor surfaces. "There's a little nurse up there in Asheville, but they won't agree for me to send for her. She takes care of people like me. She takes a hammer and knocks them in the head!"
Buck Wilson didn't have much time to talk. The jury was out, but it might not be too long before the courthouse filled back up for the verdict, and you don't have murder trials every day. But the sun was warm on the bench outside the courthouse, and he could spare a few minutes to talk about life.
Wilson never tied himself down to a factory job. Not that he didn't work hard for most of his 80 years. He raised tobacco and corn, worked at a sawmill, hauled pigs, "went many a time day and night in a truck." He did, in short, a variety of hard, dusty jobs. But factory work—that's confining, and Buck Wilson likes being on his own.
He was married once, but he and his wife parted company in 1968. She's in Illinois now, and so are his daughter and grandson. Mostly he's been on his own, but four years ago "my health went bad," and he could no longer manage by himself. Last year, he lost a leg "because of my sugar," and doctors are struggling to save the other one.
He now lives in one of the county's five family care homes with five other residents. Edwina and Boyd Mintz, with assistance from their eight-year-old daughter, Violet, run the home and provide meals and housekeeping in a family setting. The Mintz home is okay, Wilson says. "It's somewhere to sleep, three meals a day, the food's all right." The Mintzes are good people who stood by him when he was in the hospital last year.
He doesn't spend a lot of his daytime hours there. Mostly he's in downtown Marshall, taking in the action at the Madison County courthouse, talking with friends, often catching the bus to the senior nutrition site for lunch. The artificial leg slows him down some, but then there's not much reason to rush.
Edwina Mintz is taking classes to learn how to provide more planned activities, such as crafts and games, for the residents. That's kind of them, Wilson thinks, but he'd just as soon be in Marshall, coming and going as he pleases.
He enjoys being with Violet. In a way it's like having a young daughter again. They play school, with her as teacher, and she helps him take care of his remaining leg. "She's a fine little girl, that little Mintz girl. First thing I know, she'll be married and gone."
Wilson reminisces briefly about his own daughter's youth. "Maybe I'll visit her in Springfield someday," he says, and drifts back into the courtroom to join his friends.
Allen Peck is temporarily in the Madison Manor nursing home. He's been there two weeks and is working patiently at exercises as directed by the physical therapist. His patience falters, however, at silly questions, condescending attitudes, or any other inference that he isn't in control. Are they taking good care of him? "They don't have anything to do with taking care of me," he insists.
The therapist has been kidding with him, sharing jibes, making the exercise a social time for both. Her attention wanders briefly, and her movements become temporarily mechanical.
"You're not giving me anything to push against, damn it. How can I push if you don't?" says Peck. The challenge brings her back, and the kidding begins again.
The session over, Peck is wheeled into a sitting room to talk with visitors. A children's show blares unwatched on the television. Notices of upcoming activities brighten the walls, and other patients wander by. Peck is more interested in his visitor's cigarette, and asks if he has one to spare. Is he allowed to smoke in here? "I'm going to whether they like it or not."
Peck, 80, has been on his own since he was 16 or 17. He's farmed and done a number of other jobs, but now doesn't do much of anything, he says. He and his wife live about a mile up a dirt road off a paved, winding road appropriately named Grapevine. He says he'll go back "when I get good and ready."
It's lunchtime. Trays of hot meals are rolled down the halls, and a woman in white comes into the sitting room carrying a large bib. "You mind if I go ahead and put this on him?" she asks Peck's visitors as if he were not there. "It's lunchtime." She turns to Peck, "Hold up your little arms, Allen, so I won't hit that cigarette."
Peck glares, and a cough substitutes for a comment. But he submits to the bib, then sits patiently waiting for lunch.
Tags
Millie Buchanan
Millie Buchanan, 43, is a freelance writer living in Asheville, North Carolina. (1985)