This article originally appeared in Southern Exposure Vol. 6 No. 2, "Sick for Justice: Health Care and Unhealthy Conditions." Find more from that issue here.
Howard Price loves to tell visitors to Cedar Grove, West Virginia, that he’s just a “dumb coal miner.” Would that we were all so “dumb”!
An electrician by trade and a working miner, Price is also the coordinator of the Miners Committee to Save Our Clinics and the president of his community clinic, the Upper Kanawha Health Association. In the summer of 1975, he and seven friends each contributed $1.25 to incorporate the Association. By September, 1978, the paltry investment of $10 will have mushroomed to $1,000,000 to finance their vision of a community health facility.
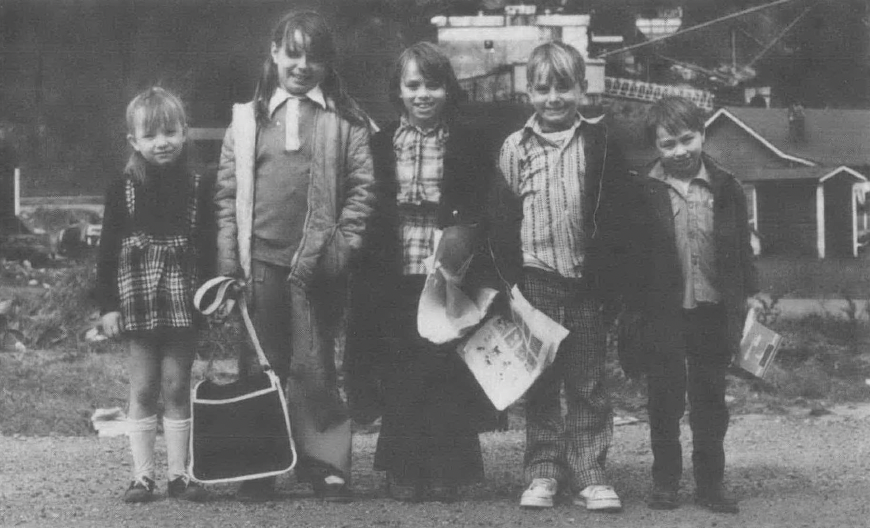
They’ve already located the clinic in a freshly painted, gold-carpeted school which they purchased with money from the federal government. The first floor of the old, neighborhood school had been almost entirely renovated for the clinic by February, 1978. But the community center atmosphere remains. The school gym is still intact, and one can generally find a basketball game or a union local meeting behind the doors which separate the gym from the clinic.
It hasn’t been easy establishing a clinic in Cedar Grove. Howard Price can remember how every nickel and dime was raised: from community rummage sales, bake sales, the Appalachian Regional Commission, the county court, private foundations, the federal government, and many neighbors and friends.
The biggest help, however, has come from the Health and Retirement Funds of the United Mine Workers, the union Price belongs to and the union that touches Grove area. Of the 9000 county residents, almost half are active or retired miners and their families. About seventy percent of the people who have visited the clinic since it opened in June, 1977, have been beneficiaries of the UMWA Health and Retirement Funds. Eight percent receive Medicare or Medicaid, and another twenty percent are either covered by private health insurance or have no insurance. No one is denied care because they can’t pay for it; but prior to the UMW Funds cutbacks in July, there was little need for “charity medicine.” The Funds made it financially possible to operate the clinic and keep it controlled by a board, seventy-five percent of whose members must be miners, according to the Association bylaws. (None of the eighteen board members are women, Price admits with embarrassment.)
It has taken more than just money to get the clinic into operation. In order to be eligible for public funds, the clinic had to first receive a “certificate of need” from the local health planning agency. The local authority pointed out that another clinic existed right across the street from the school. Housed in a trailer, the privately owned Hygeia Clinic boasted one physician on its staff. Price and other community residents were unimpressed. “After twenty years they had just one doctor,” he recalls. “That ain’t progress.”
A team of experts from Columbia University found that the Hygeia Clinic provided only curative medical treatment, made little use of nonphysician providers, and had no community control over its practices. So the Upper Kanawha Association pressed its bid for approval from the health agency - and, after a long Fight, the clinic was okayed.
The next fight was to staff the clinic with doctors from the National Health Service Corps, and once again, the clinic needed an official seal of approval. The Corps is a system which places young doctors in communities lacking adequate health care services, after these doctors have completed government-subsidized medical training. But the local medical society must approve the program before any doctor can be assigned to an area. Despite the fact that the county had only three doctors (one was over seventy), the Charleston and Upper Kanawha County Medical Societies maintained there was no need for additional doctors - and refused to allow the clinic to obtain the services of National Health Service Corps physicians.
Price and his friends took the case to higher authorities. After two years, the federal government overruled the medical society. Soon there will be a medical doctor and a dentist from the National Health Service Corps at the Cedar Grove clinic. The clinic can then provide community people with a full range of “primary care” — everything short of hospitalization. Plans for the next three years provide for increasing the staff from seven to fourteen, with all on salary and having input into daily decision-making and personnel policy. In addition to offering traditional medical care, the clinic plans to provide home health services, health education, social work, x-rays, physical therapy, nutrition services, occupational and environmental health advocacy, inhalation therapy for miners (many of whom suffer from black lung), and continuing education for the staff.
But the empire-building schemes, dear to the hearts of many professional health care administrators, make no sense to Howard Price. Asked if he wanted to purchase new equipment to provide high technology care and inpatient services, he replied: “We want the best primary care. Our machines are used. Why should our patients have to pay for expensive equipment that nobody uses?”
The Funds Die
While a sense of pride and accomplishment exudes from the staff and the community board, the battle for survival has barely begun. The first major blow was dealt barely a month after the clinic’s birth. On July 1, 1977, the UMW Health and Retirement Funds — which provide about seventy percent of the clinic’s monthly income — reversed a twenty-five-year-old tradition of commitment and support for clinics in mining communities. Upper Kanawha is only one of about fifty miners’ community clinics dependent on the Funds for their financial security.
As Helen Lewis from the Highlander Center says, “These clinics are the most progressive tools for providing health care in the area....Rural health problems include environmental and living problems such as water quality, sewage, diet, housing and occupational hazards. Community health clinics provide a local structure through which these problems can be considered.”
The Funds reimbursed the clinics through a “retainer” system, providing a percentage of the clinics’ total monthly operating costs equal to the percentage of the clinics’ clientele who are UMW Funds beneficiaries. The reimbursement procedure was based upon the clinics’ total costs — which include maintenance, staff salaries, equipment and supplies — rather than on the traditional fee-for-service formula. Thus, the clinics have been able to provide a wide range of services delivered by physician and nonphysician teams, and have been able to keep the fees low for patients who are not beneficiaries of the UMW Funds.
Fee-for-service medical practice, on the other hand, pays providers for every service they deliver; there is an incentive to provide more and more — even if it is unnecessary, wasteful, expensive, and sometimes harmful.
As of July 1, 1977, the Funds announced they were going broke and were replacing the retainer payment system with a fee-for-service system that required miners to pay the first $500 of their medical bills from their own pockets. The coal fields exploded as 80,000 miners went on wildcat strikes to protest the cuts in benefits. Howard Price formed the Miners Committee to Save Our Clinics, and some twenty clinics created the Associated Clinics of Appalachia to have a unified voice in fighting the cutbacks.
In a statement from the clinic association to the Funds on July 26, Don Conwell from the New Kensington Clinic (Pa.) explained: “By having the retainer arrangement, many areas were able to hire doctors because they could guarantee them a salary. With the withdrawal of the retainer and the ultimate collapse of these clinics, these doctors in many cases will leave and areas that are already underserved will be worse off and miners will be unable to obtain good medical care....It is mind-boggling to try to understand why the innovators of a system that they have fought for and worked for would turn away from their own concept at a time when the rest of the nation is realizing that this is the best way to go... .We plead with you, don’t take away the best and most progressive health care program in the nation and throw it into the expensive control-free fee-for-service market.”
Price, as spokesman for the Miners Committee to Save Our Clinics, appealed to Harry Huge, the union’s representative and chairman of the Funds: “You seem to think that making it difficult to see a doctor for these people will save the Funds money. Of course, it will not save money. Our children will grow up less healthy, and there will be more severe illnesses among our older people which will require more hospitalization... .Preventive health programs are being killed because they just cannot be supported on a fee-for-service basis....You have opened the gates for the rip-off artists who run patients through like cattle and thrive on your fee-for-service philosophy....You are making us pay for health care that will be harder and harder to find.”
And the Funds responded. Martin Danziger, the Funds’ administrator, wrote to Price, “Please be assured that our commitment to the clinic system is undiminished.” Harry Huge echoed, “The Funds remain committed to the outpatient care model and the prepaid clinics built around that model. There has been no change in our philosophy, nor in our long range plans.”
The miners finally went back to work after gaining a promise that the Funds’ coverage would be renegotiated.
The next blow came on December 6, 1977, the expiration date of the 1974 contract between the UMW and the Bituminous Coal Operators Association and the beginning of the longest coal mining strike in American history. All payments from the Funds to the clinic stopped, with little hope of ever being revived. The clinics were forced to lay off health workers. Medical staffs which had been developed for twenty-five years in the older clinics began to disintegrate. The process of killing the clinics was exacerbated. And people suffered. Many patients stopped all visits to the clinics. And many clinics provided medical care with little hope of ever being reimbursed.
At this writing, there is every reason to believe that the UMW Health Funds will be discontinued and replaced by private insurance companies. How will this move affect the clinics? Most insurance companies reimburse only physicians and on a fee-for-service basis. Therefore, the teams of health workers, consisting of physicians, physicians’ assistants, nurse practitioners, nutritionists, health educators and social workers, will almost surely be destroyed. Mountain communities which have had such hard times trying to attract physicians will have even harder times. And ancillary personnel won’t be eligible for reimbursement from the insurance companies. In order to maintain these health teams and their services, fees will have to be drastically increased and the clinics will enter the private, inflationary, irrational market system. Or services will be severely curtailed.
Is there any hope for the clinics’ survival? While the older, larger clinics may be able to adjust to the new situation, the prospects for the younger, smaller community clinics such as Cedar Grove are less encouraging. As long as the existence of the clinics is dependent on a single industry, their survival will continue to be tenuous. But this bleak picture of the future of the clinics assumes that there will be no change in national health policy. It assumes that the only actors on the stage are the UMW, the coal operators, and the clinics. This, clearly, is only one piece of the total federal health picture.
Although the clinics could not get special Congressional action for their own salvation, a new national health policy could dramatically affect the miners’ predicament. The Carter Administration has promised national health insurance. But “national health insurance” is a very general expression which can mean little more than the government contracting out to the private sector for the delivery of health care to some part or all of the population. It could mean little more than an expansion of the Medicare and Medicaid programs.
National health insurance, regardless of the specific program, is only a way to pay for the current health care system. It intentionally does little to change it.
The Dellums Bill
Could a national health insurance program save the clinics? Maybe. Depending on the specific legislation that would be passed by the Congress, such a program would certainly subsidize, to a lesser or greater extent, the already established clinics. But in order to support the existing clinics and build on their positive experiences by developing similar community-based health care facilities around the country, there must be a federal commitment for a national health service where communities have the money to hire health practitioners, build health centers and develop community programs according to their own needs and priorities.
As Congressman Ronald Dellums (D-Ca.) told Howard Price and the American Public Health Association last October: “It is time to begin the fight for a national health service by recognizing the most immediate needs while organizing the political support to ensure the only meaningful long-term solution.”
Dellums has introduced the Health Service Act, to create a national health service to be financed entirely out of progressive federal tax revenues. The Health Service Act would replace the entire profiteering health care industry with a system that would be publicly controlled. The United States Health Service would be a tax-supported public agency providing a complete range of health services to the entire population in publicly-owned facilities.
As envisioned in the Dellums bill, USHS has a four-tiered structure:
• At the “Community Level,” there will be primary care services — general outpatient care, emergency services, mental health care, and programs for occupational health and safety and environmental monitoring. These will be provided by community health centers and other local facilities — controlled by elected boards, consisting of two-thirds users and one-third health workers. Structures like the miners’ community clinics would provide the base of the system.
• Serving the larger “District” will be the general hospital for inpatient services. The district-level hospital will be governed by a district health board whose members will be chosen by each of the community boards.
• Several districts will join together as a “Region” to set up a specialized medical center and the health worker education system.
• The national level will supervise specialized research and overall budgeting and financing.
Controlled at every level by democratically elected boards, the Health Service will maintain strict cost and quality controls over health care, using many of the techniques demonstrated by the miners’ community clinics.
Health care will no longer be the private preserve of self-employed, self-regulated, self-selected — and entirely unaccountable - “professionals.” Instead, health care providers will be salaried workers — like you and me. Salaries will be in line with experience, education, and the nature of one’s job, and the rigid hierarchy of health care occupations will be eliminated.
For the individual user, health care will be free, just as it was for the miner and his family who carried the cherished UMW medical card. No longer will the doctor, clinic, or hospital ask the barbaric question, “How much can you pay?”
Health costs for the entire society will also be reduced. No longer will we pick up the tab for the administrative costs of insurance and billing procedure; for the unnecessary treatments and hospitalization encouraged by fee-for- service medical practice; or for excessive profits and astronomical incomes of the professional elite.
Meanwhile, unlike the present medical licensing system, the Health Service will continuously review the performance of health care personnel, with both consumers and health workers participating in the evaluations. Instead of medical schools dominating public health care facilities through affiliation contracts, as is the practice now, the Health Service will encompass the educational facilities. The new health care system will provide health workers with continuing education to maintain and improve their skills.
The Dellums Health Service Act also includes a patient’s “Bill of Rights” designed to sensitize the entire health care system to the special needs of groups which have been abused by the existing health industry.
The Bill of Rights guarantees:
• Access to all health services
• Choice of health care providers
• Advocacy and legal assistance
• Clear information and explanations, in one’s own first language, about one’s health and proposed treatments.
The principles for a national health service are already backed by the United Electrical Workers, the American Public Health Association, the Gray Panthers, the National Association of Social Workers, Rural America, and other organizations, as well as by thirty-one percent of the American public, according to the latest Harris poll.
While the reality of a national health service is still a dream, the nightmare which faces the miners’ community clinics is only too real. In building a movement for a national health service, we cannot sit by and watch the execution of the clinics’ death sentence, nor can we settle for the bureaucratic tinkering which may allow the clinics to squeak by as only shadows of their community health service potential.
The immediate hardships must be seen in a more general framework. Fighting for piecemeal reform from the government, the union, the Funds, or the operators, can, at best, ameliorate the most pressing, short-term needs. But what happens when the grant expires, the National Health Service Corps doctor moves to suburbia, the union goes out on strike, the Funds become managed by self-serving lawyers, and the companies reinstate the company doctors or use health care as a club with which to threaten coal miners, their families, and their communities?
The crisis of the miners’ community clinics represents the crisis which is being experienced in health care throughout the country. The entire country must hear and identify with the desperate cries of the Appalachian people. If not, then as Don Crowell of the Clinic Association warns, “Once again the forgotten people will be the mountain families who mine the coal that keeps this nation going.”
Tags
Joyce Goldstein
Joyce Goldstein is the executive director of Health Service Action, a group organizing for national health service and in support of local struggles to build community-controlled health care facilities. It is headquartered in Washington and has affiliates in several states and cities across the country. Local and statewide health service advocacy groups are forming in Illinois, Pennsylvania, California, New York, New Jersey, and Washington, D.C. (1978)